The effects of the EED on Left Ventricular and Arterial Pressures
The circulatory effects of application of the EED can be summarized by using the typical cardiac cycle diagram shown above. In this diagram the pressure inside the left ventricle axis is seen (in brown or gray) to increase rapidly at the beginning of the Systole, peak and then fall to near zero pressure. During the Diastole the ventricular pressure increases gradually as the ventricle fills with blood.
The pressure in the aorta and the large arteries follows the ventricular pressure once the aortic valve opens and the rapid ejection starts. The aortic pressure contintues to follow the ventricular pressure until the aortic valve closes. In normal circulation the aortic pressure falls gradually as more and more blood is supplied to the organs and tissues during the Diasotle (orange line in diagram). The rate of diastolic pressure fall is influenced by the resistance of the arteries and arterioles that lead to the organs and tissues. This resistance, called Systemic Vascular Resistance - SVR. The rate of diastolic pressure fall is also dependent on the cardiac output. If the cardiac output is low, or when the SVR is reduced as may happen in shock or during CPR, the pressure during diastole falls much faster than normal as shown by the light blue line.
Changes in the Diagram when the EED is used.
When the EED is used it pushes blood from the limbs (legs usually) to the center. This blood increases the venous return to the heart so that the filling of the left ventricle is improved and the ventricular filling pressure incline during Diastole is steeper (brown line marked as B). This increased ventricular filling increases the End-Diastolic Volume EDV of the ventricle, which, through the Frank-Starling mechanism, increases ventricular contractility, stroke volume and cardiac output. However, the EED has a second effect: it blocks the arterial flow into the limbs the EED is placed on. This effect of the EED impedes the flow out of the aorta to the limbs and has an immediate and direct effect on the SVR. Both effects (increased cardiac output and increased SVR) reduce the rate of fall of pressure in the aorta and main areteries during Diastole as shown schematically in the green line marked as A.
In summary, the overall physiological effects of applying the EED on a patient are:
1. Increased Venous Return to the heart
2. Increased Stroke Volume
Resulting in:
3. Increased systolic blood pressure
4. Increased diastolic blood pressure
Increasing diatoslic blood pressure increases the coronary arteries perfusion since the blood supply to the cardiac muscle is predominantly during diastole.
The use of the EED also reduces the ratio of unstressed to stress vascular volume (What is this???).
The circulatory effects of application of the EED can be summarized by using the typical cardiac cycle diagram shown above. In this diagram the pressure inside the left ventricle axis is seen (in brown or gray) to increase rapidly at the beginning of the Systole, peak and then fall to near zero pressure. During the Diastole the ventricular pressure increases gradually as the ventricle fills with blood.
The pressure in the aorta and the large arteries follows the ventricular pressure once the aortic valve opens and the rapid ejection starts. The aortic pressure contintues to follow the ventricular pressure until the aortic valve closes. In normal circulation the aortic pressure falls gradually as more and more blood is supplied to the organs and tissues during the Diasotle (orange line in diagram). The rate of diastolic pressure fall is influenced by the resistance of the arteries and arterioles that lead to the organs and tissues. This resistance, called Systemic Vascular Resistance - SVR. The rate of diastolic pressure fall is also dependent on the cardiac output. If the cardiac output is low, or when the SVR is reduced as may happen in shock or during CPR, the pressure during diastole falls much faster than normal as shown by the light blue line.
Changes in the Diagram when the EED is used.
When the EED is used it pushes blood from the limbs (legs usually) to the center. This blood increases the venous return to the heart so that the filling of the left ventricle is improved and the ventricular filling pressure incline during Diastole is steeper (brown line marked as B). This increased ventricular filling increases the End-Diastolic Volume EDV of the ventricle, which, through the Frank-Starling mechanism, increases ventricular contractility, stroke volume and cardiac output. However, the EED has a second effect: it blocks the arterial flow into the limbs the EED is placed on. This effect of the EED impedes the flow out of the aorta to the limbs and has an immediate and direct effect on the SVR. Both effects (increased cardiac output and increased SVR) reduce the rate of fall of pressure in the aorta and main areteries during Diastole as shown schematically in the green line marked as A.
In summary, the overall physiological effects of applying the EED on a patient are:
1. Increased Venous Return to the heart
2. Increased Stroke Volume
Resulting in:
3. Increased systolic blood pressure
4. Increased diastolic blood pressure
Increasing diatoslic blood pressure increases the coronary arteries perfusion since the blood supply to the cardiac muscle is predominantly during diastole.
The use of the EED also reduces the ratio of unstressed to stress vascular volume (What is this???).
The Red Balloon model of the EED effect on the unstressed/stressed volume ratio
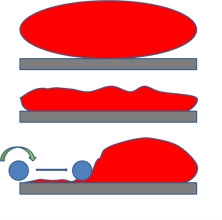
When both blood volume and vascular volume are normal the circulatory pressure is maintained. This is depicted in the nicely stretched oval balloon in the top of the diagram on the left.
When blood volume falls (e.g. due to hemorrhage or dehydration) or the volume of the blood vessels becomes pathologically large (e.g. due to sepsis, anaphylaxis, or drugs), the pressure in the system falls and the balloon "sags".
Rolling the EED (symbolized by the blue roller) over one part of the system (e.g. legs) and squeezing its content (blood) into the other part of the system (e.g. the central circulation) increases the pressure and stretches the latter. This, in fact, reduces the ratio of the unstressed to stressed volume in this part of the circulation.
When blood volume falls (e.g. due to hemorrhage or dehydration) or the volume of the blood vessels becomes pathologically large (e.g. due to sepsis, anaphylaxis, or drugs), the pressure in the system falls and the balloon "sags".
Rolling the EED (symbolized by the blue roller) over one part of the system (e.g. legs) and squeezing its content (blood) into the other part of the system (e.g. the central circulation) increases the pressure and stretches the latter. This, in fact, reduces the ratio of the unstressed to stressed volume in this part of the circulation.
Physiological effects of the EED in hemodynamic shock
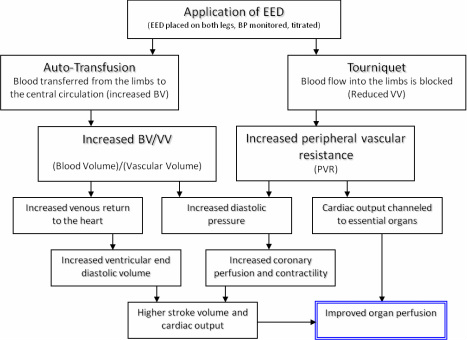
The rolling up of the EED on a limb displaces blood to the central circulation. This is in fact a form of "Auto-Transfusion" of the patient's own blood (no risk of mismatch), in essentially the right temperature, with all of the needed clotting factors and oxygen carrying capacity (stored blood is anticoagulated, cold and depleted of 2,3,DPG which shift the O2-Hemogobine Dissociation Curve to the left thereby reducing it ability to tranport oxygen to the tissues). The auto-transfusion effect increases the Blood Volume BV in the Central Circulation. The EED ring occludes arterial inflow into the limb, acting as a Tourniquet. By doing so, it increases the Peripheral/Systemic Vascular Resistance (PVR or SVR) and limits or reduces the Vascular Volume VV in which the patient's Blood Volume resides. The ratio BV/VV in the central circulation is increaseed, venous return to the heart rises so that the ventricular filling and end diastolic volume EDV is higher, leading to a greater stroke volume and cardiac output. The higher diastolic pressure helps heart muscle perfusion via the coronary arteries, which further helps with cardiac performance. The overall result is an improvement in organ perfusion. The blocking of bloodflow to the limbs does not result in ischemic injury provided that the duration is limited to 120 minutes (see section on extending EED ischemia duration).
Physiological effects of the EED during CPR in circulatory (cardiac) arrest
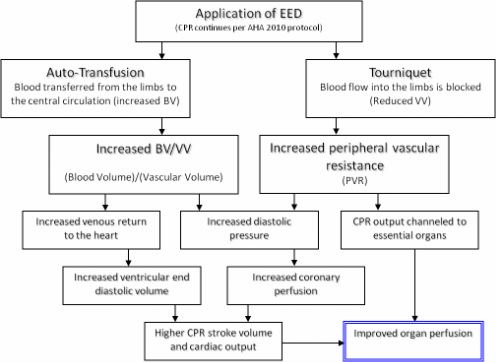
External Chest Compression is a key component in CPR and the sole means of creating cardiac output when effective spontaneous contractions are stopped. However, even when expertly done, manually or by a machine, external chest compression results in no more than 25-30% of the patient's normal cardiac output. The systolic blood pressure reaches 70-80 mm Hg and the diastolic pressure is not more than 20 mm Hg (see Hemodynamics during CPR Bibliography). It is now accepted that the main reason for these low values is the very low venous return of blood to the heart. This is caused by the loss of sympathetic tone that occurs almost as soon as blood flow to the brain is stopped. The blood vessels all around dilate and the blood pools in the periphery. (In fact, the main reason for using adrenalin and vasopressin during CPR is to counteract this extreme vasodilatation). Clearly, if blood is not returning to the heart, the chambers do not get filled and as such, even if compressed very firmly, will not generate output. Bringing blood from the periphery to the heart is critical. In recent years, a range of devices has been introduced to the emergency market with the intent to "suck" blood from the periphery to the chest. These include the Plunger method and its variants and the inspiratory threshhold devices.
When the EED is used during CPR it has two distinct functions: It compresses the blood vessels in the limbs acting like a "mechanical vasoconstricotr" of sort. It also blocks blood supply to the legs so that the generated cardiac output is channeled to the essential organs. In addition, the increased PVR/SVR helps boost the diastolic blood pressure in the aorta which is key to effective coronary perfusion.
When the EED is used during CPR it has two distinct functions: It compresses the blood vessels in the limbs acting like a "mechanical vasoconstricotr" of sort. It also blocks blood supply to the legs so that the generated cardiac output is channeled to the essential organs. In addition, the increased PVR/SVR helps boost the diastolic blood pressure in the aorta which is key to effective coronary perfusion.
Hemadynamics during CPR Bibliography
Del Guercio LMR, Coomaraswany R, State D: Cardiac output and other hemodynamic variables during external massage in man. N Engl J Med 1963; 269: 1398.
Jackson RE, Freeman SB: Hemodynamics of cardiac massage. Emerg Med Clin North Am 1983; 1: 501.
Luce JM, Ross BK, O'Quinn, et al: Regional blood flow during cardiopulmonary resuscitation in dogs using simultaneous and nonsimultaneous compression and ventilation. Circulation 1983; 67: 258.
Maier GW, Tyson GS, Olsen CO, et al: The physiology of external cardiac massage: High-impulse cardiopulmonary resuscitation. Circulation 1984; 70: 86.
Paradis NA, Martin GB, Goetting MG, et al: Simultaneous aortic, jugular bulb, and right atrial pressures during cardiopulmonary resuscitation in
humans: Insight into mechanisms. Circulation 1989; 80: 361.
Ditchey RV, Winkler JV, Rhodes CA: Relative lack of coronary blood flow during closed chest resuscitation in dogs. Circulation 1982; 66: 297.
Niemann J, Rosborough J, Ung S, et al: Coronary perfusion pressure during experimental cardiopulmonary resuscitation. Ann Emerg Med 1982; 11: 127.
Sanders AB, Ogle M, Ewy GA: Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med 1985; 3: 11.
Jackson RE, Freeman SB: Hemodynamics of cardiac massage. Emerg Med Clin North Am 1983; 1: 501.
Luce JM, Ross BK, O'Quinn, et al: Regional blood flow during cardiopulmonary resuscitation in dogs using simultaneous and nonsimultaneous compression and ventilation. Circulation 1983; 67: 258.
Maier GW, Tyson GS, Olsen CO, et al: The physiology of external cardiac massage: High-impulse cardiopulmonary resuscitation. Circulation 1984; 70: 86.
Paradis NA, Martin GB, Goetting MG, et al: Simultaneous aortic, jugular bulb, and right atrial pressures during cardiopulmonary resuscitation in
humans: Insight into mechanisms. Circulation 1989; 80: 361.
Ditchey RV, Winkler JV, Rhodes CA: Relative lack of coronary blood flow during closed chest resuscitation in dogs. Circulation 1982; 66: 297.
Niemann J, Rosborough J, Ung S, et al: Coronary perfusion pressure during experimental cardiopulmonary resuscitation. Ann Emerg Med 1982; 11: 127.
Sanders AB, Ogle M, Ewy GA: Coronary perfusion pressure during cardiopulmonary resuscitation. Am J Emerg Med 1985; 3: 11.
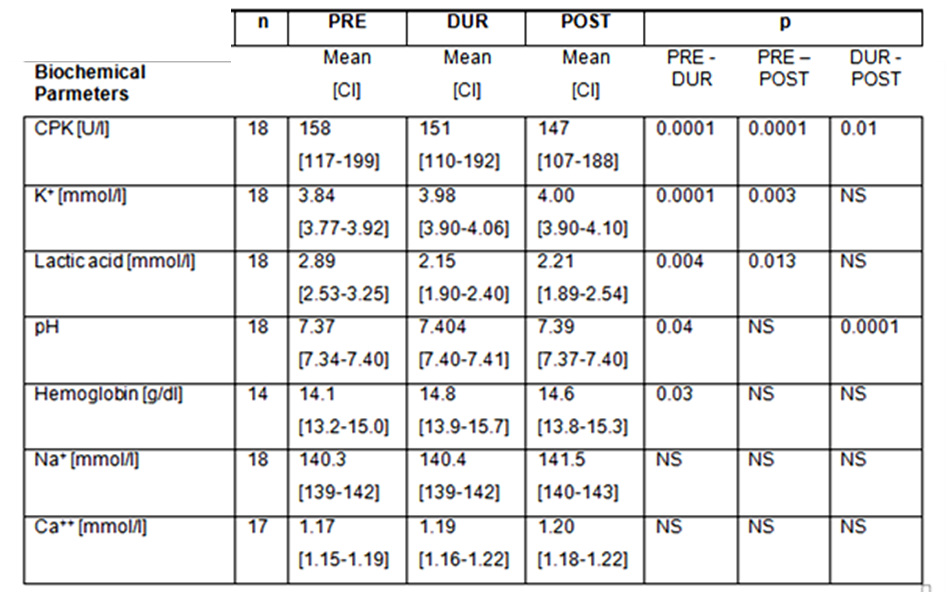
Summary of EED (A-TT) physiological study
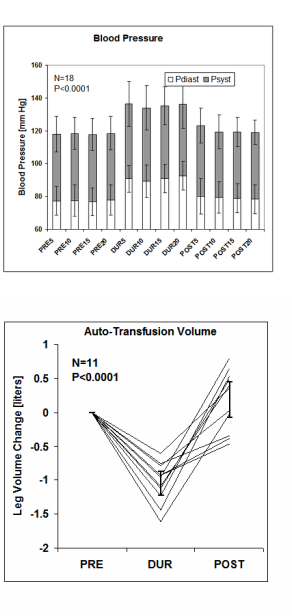
The physiological and biochemical effects of A-TT on 18 normal volunteers were assessed by applying the A-TT device on them for 20 minutes. It was observed that A-TT gave rise to 17.4; (14.5-20.3) (Mean; (CI)) and 13.1; (11.0-15.1) mm Hg rise in systolic and diastolic blood pressures, respectively (P < 0.0001) Figure 1. The leg volume dropped by 1040 ml; (863-1216) ml during A-TT application (P < 0.0001) Figure 2. Ventilation and gas exchange parameters did not change except for a slight rise in Sp O2(P < 0.001) Table 1. There was a statistically significant decline in creatinine phosphokinase (CPK) and lactic acid, with no change in Ca++ and Na+ concentrations Table 2. The authors concluded that A-TT indeed induces significant auto-transfusion and blood pressure elevation in normal volunteers. [1] Moreover the biochemical data indicated that applying the A-TT did not cause significant deleterious tissue ischemia or mechanical crush injury.
A-TT (Auto - Transfusion Tourniquet) is the generic name of the EED by OHK.
From: Fatimah Lateef and Tan Kelvin, J Emerg Trauma Shock. 2008 Jul-Dec; 1(2): 63–69.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700619/
1. Oren G, Tov N, Aharon S, Yael S, Noam G. Rappaport, Technion. Haifa: Israel Institute of echnology; 2000. Auto transfusion and blood pressure elevation by elastic leg compression in normal subjects.
A-TT (Auto - Transfusion Tourniquet) is the generic name of the EED by OHK.
From: Fatimah Lateef and Tan Kelvin, J Emerg Trauma Shock. 2008 Jul-Dec; 1(2): 63–69.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700619/
1. Oren G, Tov N, Aharon S, Yael S, Noam G. Rappaport, Technion. Haifa: Israel Institute of echnology; 2000. Auto transfusion and blood pressure elevation by elastic leg compression in normal subjects.